Decoding your gut ...
Do we need another epidemic? The chronic disease epidemic … heart disease, cancer, and diabetes has been with us for some time and continues, as has the obesity epidemic. Who can forget coronavirus … Covid … another epidemic that keeps on giving. Gut issues, that is, health problems with our digestive system, that long tube between our mouth and our anus including our stomach and intestines, have been with us for some time but seemingly more talked about today. Combined, about half of the US population suffers from at least one chronic disease. Holman, H., “The Relation of the Chronic Disease Epidemic to the Health Care Crisis,” ACR Open Rheumatol 2(3):167-173 (Mar 2020). https://doi.org/10.1002/acr2.11114
The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) reported in 2022 that 60 to 70 million people in the US suffer from gastrointestinal (GI) diseases, about twenty percent of the US population. These sufferers generate about 100 million ambulatory care visits to medical facilities per year. Uncounted are the people who try over-the-counter digestive aids before seeking medical advice, e.g., those taking Mylanta, TUMS, Rolaids, Alka-Seltzer, PepcidAC, Tagamet HB 200, Prilosec OTC, Nexium, or Prevacid. National Institute of Diabetes and Digestive and Kidney Diseases, “Digestive Diseases Statistics for the United States.” https://www.niddk.nih.gov/health-information/health-statistics/digestive-diseases; Almario, C., et al., “Burden of Gastrointestinal Symptoms in the United States: Results of a Nationally Representative Survey of Over 71,000 Americans,” Am J Gastro 113(11):1701-1710 (Nov 2018). https://doi.org/10.1038/s41395-018-0256-8 A poll conducted in May 2023 found that “most Americans are uninformed about the gut microbiome and its impact on general health and well-being.” https://www.ipsos.com/en-us/most-americans-are-uninformed-about-gut-health-and-microbiome As you should anticipate, gut issues are also increasing worldwide. Wang, R., et al., “Global, regional, and national burden of 10 digestive diseases in 204 countries and territories from 1990 to 2019,” Front Public Health 11:1061453 (Mar 28, 2023). https://doi.org/10.3389/fpubh.2023.1061453
Why are so many of us suffering gastrointestinal distress? Scientists agree there are at least four major drivers of gut issues: lifestyle issues such as stress, traumatic experiences and lack of social support; overuse of antibiotics; pesticides; and a diet of ultra-processed foods. Now we can add irregular sleep to the list of gut issue drivers.
“When we ingest 60 percent of our calories from ultra-processed foods, as most Americans do, we destroy our microbiome (i.e., the ecosystem in our gut). The microbiome plays a role in every disease, so why aren’t we doing more to protect and restore it? One third to one half of all Americans have gut issues due to the constant consumption of industrialized foods, glyphosate, food additives, and more. This is a problem—and it’s time for us to take action.” Dr. Mark Hyman, “Why Gut Issues Are On The Rise And How To Fix It,” Episode 556, The Doctor’s Farmacy (Jun 17, 2022). https://drhyman.com/blog/2022/06/17/podcast-ep556/
Stress really needs no explanation … we all experience it on a daily basis. It comes in many forms … pressure to do things or pressure not to do things, financial stress, physical pain, emotional stress, lack of sufficient quality sleep, to name but a few large categories of stress. When we internalize these stresses, they go straight to our gut. Correspondingly, when we take measures to reduce stress, we benefit our gut. Harvard Health Publishing, “Stress and the sensitive gut” (Aug 21, 2019). https://www.health.harvard.edu/newsletter_article/stress-and-the-sensitive-gut
Antibiotics have been in use for ages and have served us well in treating infectious diseases and helping check infections associated with other medical treatments, for example, post-surgical. The first antibiotic, salvarsan, was used starting in 1910. Over the ensuing decade the average human lifespan has increased by 23 years. Hutchings, M., A. Truman, & B. Wilkinson, “Antibiotics: past, present and future,” Curr Opin Microbiol 51:72-80 (Oct 2019). https://doi.org/10.1016/j.mib.2019.10.008; Cook, M. & G. Wright, “The past, present, and future of antibiotics,” Sci Transl Med 14:657 (Aug 10, 2022). https://doi.org/10.1126/scitranslmed.abo7793
Unfortunately, in our “we have a pill for that” medical system, we have experienced widespread overuse of antibiotics. In a podcast on The Proof with Simon Hill, The Double-Edged Sword: Understanding Antibiotics and Your Gut Microbiome, EP271, Dr. Will Bulsiewicz, gastroenterologist and cookbook author, explained, "There are three main things that happen within the microbiome when you take antibiotics. One, a loss of diversity. Two, you are causing widespread damage to the species. And three, you are choosing and selecting the resistance microbes."
In other words, you end up with fewer species of good microbes in your gut that are less effective in protecting against pathogens, and which can develop a resistance to the positive effects of antibiotics. The microbes become resistant to the beneficial effects of the antibiotics. Yang, L., et al., “The varying effects of antibiotics on gut microbiota,” AMB Express 11(1):116 (Aug 16, 2021). https://doi.org/10.1186/s13568-021-01274-w; Konstantinidis, T., et al., “Effects of Antibiotics upon the Gut Microbiome: A Review of the Literature,” Biomedicines 8(11):502 (Nov. 16, 2020). https://doi.org/10.3390/biomedicines8110502
To make matters worse, the widespread use of antibiotics in industrial agriculture is another pathway into our guts through the food we eat. Francino, M., “Antibiotics and the Human Gut Microbiome: Dysbioses and Accumulation of Resistances,” Front Microbiol 6:1543 (Jan 12, 2016). https://doi.org/10.3389/fmicb.2015.01543; Manyi-Loh, C., et al., “Antibiotic Use in Agriculture and Its Consequential Resistance in Environmental Sources: Potential Public Health Implications,” Molecules 23(4):795 (Mar 30, 2018). https://doi.org/10.3390/molecules23040795
For example, since the 1950s antibiotics, primarily oxytetracycline and streptomycin, have been used to control some bacterial disease in high-value fruit and vegetable plants. McManus, P., et al., “Antibiotic use in plant agriculture,” Annu Rev Phytopathol 40:443-65 (2002). https://doi.org/10.1146/annurev.phyto.40.120301.093927 In dairy farming, mastitis treatment, that is, treatment of an inflammation of the mammary gland, is the most common reason for use of antibiotics. Farrell, S., et al., “Factors influencing dairy farmers’ antibiotic use: An application of the COM-B model,” J Dairy Sci 106(6):4059-4071 (Jun 2023). https://doi.org/10.3168/jds.2022-22263
Because of industrial agriculture, Americans are exposed to more pesticides and synthetic fertilizers than people in other countries. The term “pesticides” comprises herbicides, insecticides, and fungicides. These pesticides in food and water get into our gut and cause dysbiosis, an imbalance of the intestinal microbiota, and leaky gut, a condition wherein the intestinal wall is permeable and allows pathogens to pass from the intestine into the blood stream. Giambò. F., et al., “Toxicology and Microbiota: How Do Pesticides Influence Gut Microbiota? A Review,” Int J Environ Res Public Health18(11):5510 (May 21, 2021). https://doi.org/10.3390/ijerph18115510; Zhou, M. & J. Zhao, “A Review on the Health Effects of Pesticides Based on Host Gut Microbiome and Metabolomics,” Front Mol Biosci 8:632955 (Feb 8, 2021). https://doi.org/10.3389/fmolb.2021.632955; Sharma, T., et al., “Gut microbiota: a non-target victim of pesticide-induced toxicity,” Gut Microbes 15(1):2187578 (Jan-Dec 2023). https://doi.org/10.1080/19490976.2023.2187578
The standard American diet is, however, the most common culprit of gastrointestinal dysbiosis, weakened immune functioning, chronic inflammation, and disease. Too many refined carbohydrates, refined flour and sugar, and food additives, to which we add the seemingly unlimited number of ultra-processed meals (the ones you find the frozen food lockers and the center aisles of the grocery store). Belizário, J. & J. Faintuch, “Microbiome and Gut Dysbiosis,” Exp Suppl 109:459-476 (2018). https://doi.org/10.1007/978-3-319-74932-7_13; Srour, B., et al., “Ultra-processed foods and human health: from epidemiological evidence to mechanistic insights,” Lancet: Gastro & Hepa 7(12):1128-1140 (Dec 2022). https://doi.org/10.1016/S2468-1253(22)00169-8; Youmshajekian, L., “How Do Ultraprocessed Foods Affect Your Health?” Sci Am (Nov 8, 2023). https://www.scientificamerican.com/article/how-do-ultraprocessed-foods-affect-your-health/ Want to help your gut, only shop on the edges of the grocery store. That’s where you will find real food, not Frankenfood.
Recent studies have shown there is a strong association between low quality or lack of sleep and gastrointestinal diseases. Sleep deprivation can impact gut microbes after just two days of insufficient sleep. Sleep deprivation also works to increase inflammation and stress hormones in the body. Khanijow, V., et al., “Sleep Dysfunction and Gastrointestinal Diseases,” Gastroenterol Hepatol (NY) 11(12):817-25 (Dec 2015); Smith, R., et al., “Gut microbiome diversity is associated with sleep physiology in humans,” PLoS One 14(10):e0222394 (Oct 7, 2019). https://doi.org/10.1371/journal.pone.0222394
We experience conditions that give us indications about the health of our gut … abdominal pain, cramping, burping, gas, bloating, heartburn, acid reflux, flatulence, diarrhea, bloody or mucus-type stools, constipation, weight gain or loss, and fatigue. There are several tests that can directly tell us a great deal about the state of our gut and how we react to foods. Unfortunately, most of these tests are not covered by health insurance.
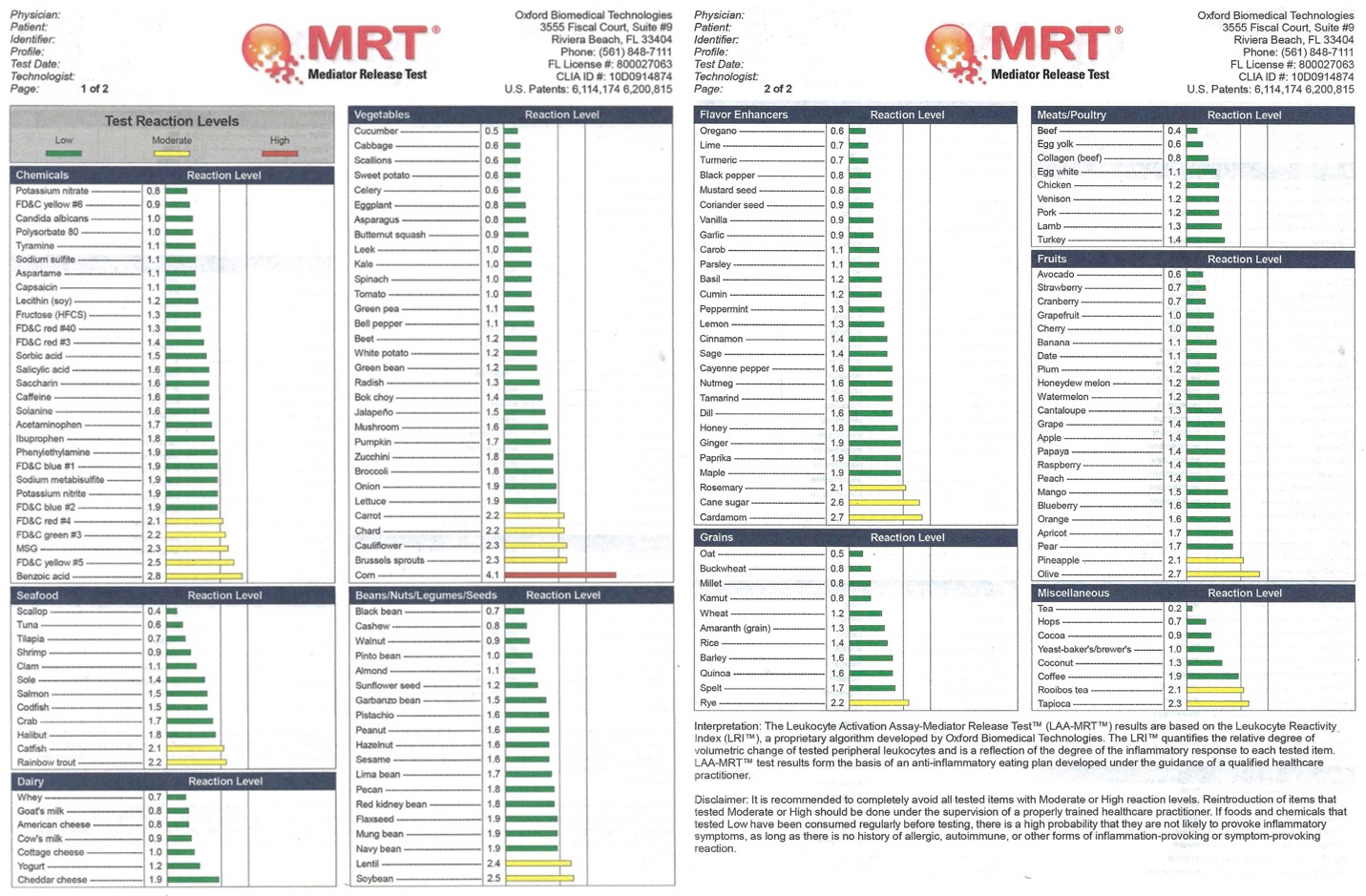
The Leukocyte Activation Assay-Mediator Release Test (MRT) is a blood test of our inflammatory response to foods. Leukocytes are white blood cells that help your body fight germs. This test looks at how the individual foods you eat trigger inflammation. Your blood sample is sent to a laboratory for testing. What you get back from the laboratory is a diagram showing the inflammatory response of your gut to foods … green, yellow or red. You should not eat red foods and go easy on the yellow ones.
There is also a numeric value associated with each food that indicates it relative inflammatory effect on your gut. In the diagram below, of vegetables cucumber has the lowest reaction level green 0.5 and corn red 4.1, do not eat. Carrots are yellow 2.2. For fruits, avocado is green 0.6 while olives are yellow 2.7. The yellow for olives also indicates olive oil should be used sparingly. All meats are green, ranging from 0.4 for beef to 1.4 for turkey; as are all dairy. Spices are interesting; oregano is green 0.6 but rosemary is yellow 2.1. Cane sugar is yellow 2.6.
Garcia-Martinez, I., et al., “A leukocyte activation test identifies food items which induce release of DNA by innate immune peripheral blood leucocytes,” Nutr Metab (Lond) 15:26 (Apr 11, 2018). https://doi.org/10.1186/s12986-018-0260-4; Mullin, G., et al., “Testing for food reactions: the good, the bad, and the ugly,” Nutr Clin Pract 25(2):192-8 (Apr 2010). https://doi.org/10.1177/0884533610362696
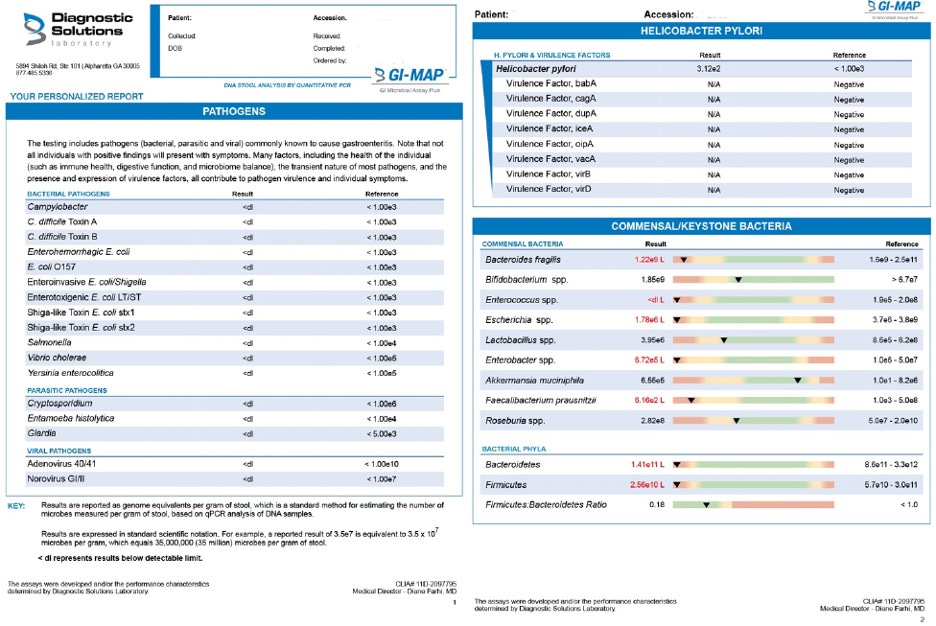
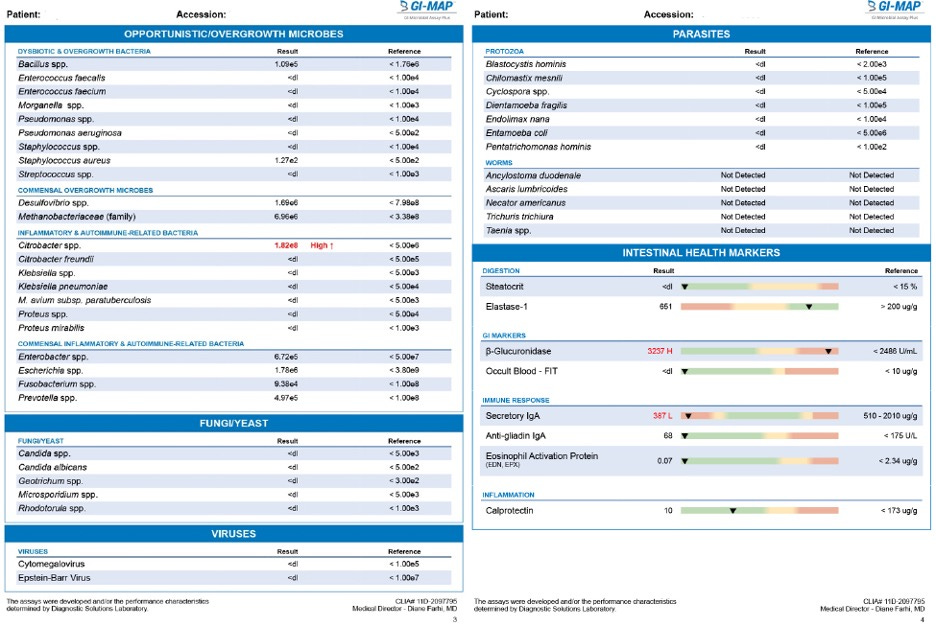
Another test, the GI-MAP (GI-Microbial Assay Plus), gives a quantitative assessment of the state of your intestinal track. A stool sample is sent to the laboratory for analysis. GI-MAP tests for gastrointestinal pathogens, opportunistic organisms, normal flora, and markers of GI health, including bacteria, viruses, parasites, fungi, inflammation, immune function, pancreatic function, and fecal occult blood. GI-MAP also assesses H. pylori antibiotic resistance genes, as well as the virulence factors associateh the pathogenicity of H. pylori. You receive in return a detailed report on what is living in your gut. The report shown below is divided into sections: pathogens, H. pylori and virulence factors, keystone bacteria, opportunistic microbes including inflammatory and auto-immune related bacteria, fungi/yeast, viruses, parasites, and finally overall intestinal health markets. The red/yellow/green bar charts are visually easy to understand, but, frankly, you need a functional or integrative health practitioner to interpret the results. Such a practitioner can use the GI-MAP to help you repair and maintain a healthy gut.
Want a healthy gut … the formula seems straight forward … pay attention to your lifestyle, avoid antibiotics to the fullest extent you can, eat only organic and non-GMO foods, preferably locally sourced. Easy to say, takes work to do. Good luck, and happy gut.







Pretty serious article there Richard. One of the things I like to use is Kefir. Specifically Ryazhenka.